A fever in a child is one of the most common types of immunological dysfunctions they experience, and it is important that the issue is taken care of correctly.
In this article we will cover what a normal temperature for a child should be, when is it tolerable for them and when it really does require medical attention.
To what degree does it need attention, and we will compare these numerical values to the normal temperature levels of adults to get a more clear picture of how to measure the child’s temperature for symptoms of fever. Where you may want to stock up on these.*
We will also cover thermometer devices in general (the instrument with which the temperature is measured), such as this* and how you should read the result after the measurement process (considering both digital and glass non-digital options).
I hope that the information that I will provide you will prove useful, and will educate and encourage regular and correct readings.
Fevers shouldn’t be taking lightly, and I hope this goes some way to help you identify fever symptoms in your child, including when to seek proper medical assistance.
Let’s get started!
What should a child’s normal temperature be?
Normal temperature for children is roughly around 36.4C (or 97.5F), albeit it can vary slightly up or down. Anything above by a significant margin is considered a fever.
Reliable symptoms by which you can recognise a fever are when their skin is hotter on touch than usual on their forehead, back or stomach.
If you have suspicions that your child’s temperature is not at normal levels, you can use a reliable thermometer to confirm the case.
If the thermometer shows temperature levels higher than 37.5C (99.5F), measured either orally (mouth) or rectally (in the bottom), then your child is suffering from a fever.
A fever can be considered any body temperature above the normal previously mentioned numbers, from a medical standpoint, a significant fever is not diagnosed until the temperature rises above 38C (100.4F).
Any less intensive forms of fever at infants are considered beneficial as they in a way “train” the immune system from an early age to fight off body infections.
Fever happens when something is going wrong in the body, usually an infection within, and the hypothalamus of the brain increases the temperature of the body to fight off the infections.
A fever can occur as well when the child is exhausted from either too much physical exercise or heat exhaustion.
What is a normal Temperature for a baby?
An infant’s normal body temperature is roughly 37C (97F to 100F).
These numbers are at our disposal due to the insight of the American Academy of Pediatrics (AAP).
If your infant’s temperature (which you have presumably determined with a thermometer) is higher than 38C for more than 24 hours, the chances are high that it’s experiencing a fever.
A fever is a sign of an underlying illness, usually an infection within the body.
If your baby is three months old or younger, fever is a serious thing to consider and a legitimate reason to be worried about. If the infant experiences a temperature of 100.4F or higher, the state is considered a medical emergency.
In that case, you are highly advised to contact your baby’s doctor, inform him of the situation and accent when informing him that the baby is three months or younger.
The proper medical attention which your baby should immediately help resolve this emergency quickly.
What is a dangerous fever for an infant, toddler or older child?
A child who is older than six months, but younger than a year having a temperature of 103F or higher or has had any level of intensity of fever for more than 24h is considered dangerous.
A child between the age of one year and two years old with any fever lasting more than 24 hours is considered dangerous too.
A child of any age with a fever of 104F or higher is considered dangerous.
In children of age under five years, a temperature higher than 37C (99.5F) is considered a fever and dangerous.
It needs to be noted that children do not have a strengthened immune system, so a fever in children under the age of 5 is very common. More than 2/3 of the parents of children younger than the age of five have reported that their child has experienced a fever at least once up to that point in its life.
From a safety point of view, a fever can be considered any elevated body temperature above the normal 37C(98.6F), albeit from a medical point of view a fever is not diagnosed (at least not an emergency situation) unless the temperature of the body is above 38C (100.4F).
Lower degrees of elevated body temperature (or less intensive fevers, simply put) are considered beneficial, have shown to cause no problems and help the body boost its immune system to fight off current and further incoming infections.
Most healthy children and adults alike can tolerate a fever as high as 39.4C (103F) to 40C (104F) for short periods of time without any problems.
Children are predisposed to have more frequent and higher intensity fevers than their adult counterparts.
Let’s Look at normal Temperatures for adults in comparison
Body temperature is the body’s way of making or getting rid of excess heat. The body is very effective in keeping its temperature stable (homeostasis) despite the changes of the temperature in the outside environment.
- When your body temperature is too high, the blood vessels in your skin widen so the heat can be carried to the surface of the skin. When the heat reaches the surface, you start to sweat, the heat evaporates, and the temperature returns to normal levels.
- On the contrary, when your body temperature is too low or you’re cold in other words, the blood vessels narrow.
Normal Human Temperature Table in Celsius
| Age Group | 1-2 | 3-10 | 11-65 | >65 |
| Oral | N/A | 35.5 – 37.5 | 36.4 – 37.5 | 35.7 – 36.9 |
| Rectal | 36.6 – 38 | 36.6 – 38 | 37 – 38.1 | 36.2 – 37.3 |
| Axillary | 34.7 – 37.3 | 35.8 – 36.7 | 35.2 – 36.8 | 35.5 – 36.3 |
| Ear | 36.4 – 38 | 36.1 – 37.7 | 35.8 – 37 | 35.7 – 37.5 |
| Core | 36.4 – 37.7 | 36.4 – 37.7 | 36.8 – 37.8 | 35.8 – 37.1 |
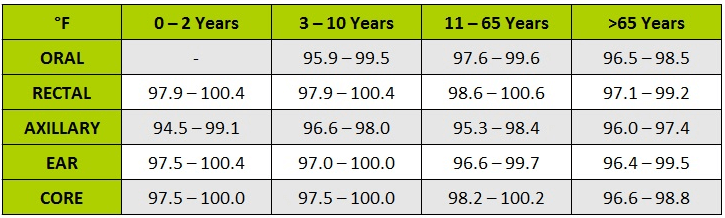
Normal Human Temperature Table In Fahrenheit
| Age Group | 1-2 | 3-10 | 11-65 | >65 |
| Oral | N/A | 95.9 – 99.5 | 97.6 – 99.6 | 96.4 – 98.5 |
| Rectal | 97.9 – 100.4 | 97.9 – 100.4 | 98.6 – 100.6 | 97.1 – 99.2 |
| Axillary | 94.5 – 99.1 | 96.6 – 98 | 95.3 – 98.4 | 96 – 97.4 |
| Ear | 97.5 – 100.4 | 97 – 100 | 96.6 – 99.7 | 96.4 – 99.5 |
| Core | 36.4 – 37.7 | 97.5 – 100 | 98.2 – 100.2 | 96.6 – 98.8 |
This reduces the flow of blood to the surface of the skin, saving body heat usually followed by shivering. By shivering the muscles start generating heat which helps you achieve normal body temperature again.
Temperatures are measured by a thermometer and can be read in a variety of ways: via the ear, the armpit, orally, rectally and so forth.
It is widely accepted that normal body temperature, measured orally (by mouth) is 37C (98.6F).
This is an average body temperature for humans.
The actual normal body temperature can be 0.6C (1F) higher or lower in actuality.
The normal body temperature can also change throughout the day depending on how physically active you are and how hot or cold the environment is.
Body temperature is also sensitive to hormone levels, so a woman is ovulating or having her period can have higher or lower body temperature compared to the numbers previously mentioned.
In the majority of adults, a fever is diagnosed when the body temperature is higher than 38C (100.4F) measured orally or 38.5C (101.3F) measured rectally or by ear.
As a comparison, a child has a fever when it’s rectal temperature is 38C (100.4F) or higher, or armpit temperature of 37.6C (99.7) or higher.
A fever occurs due to different factors, such as:
- Infections are the most common cause of a fever. The infection can be local or global to the body.
- Medicine, injury or medical condition induced fevers which are more severe and require more intensive and specialized medical attention.
How to measure your child’s temperature
The most accurate temperature* measurement method is the rectal one.
If the child is older than three months, the oral measurement method can be sufficiently accurate as well.
Digital thermometers are preferred and regarded as better.
Things to note while measuring the body temperature with a thermometer:
- Label different thermometers for their according to use, so you don’t use the rectal one in an oral measurement method for an example.
- Be sure that the thermometer which you are using is clean.
- If you measure the temperature orally, wait at least half an hour if the child has eaten or has drunk anything beforehand.
- Taking temperature after a bath is considered an inefficient method.
Don’t leave the infant alone with the thermometer.
- After done using the thermometer, be sure to clean it and if necessary, disinfect it.
If you’re taking your child’s temperature rectally, the appropriate approach would be to place it belly-down across your lap.
The tip should be coated with a lubricant before being inserted into the butt.
At any point of resistance, stop the procedure and simply hold the thermometer in place. After the procedure is done you should remove and take its reading
If the method which you are going to be using is oral measurement, the proper way to do it is o place the end of the thermometer under the infant’s tongue. The infant should place its lips softly upon the thermometer.
Have a look at our best thermometer for toddlers 2018 reviews. After that, you can take it out and do the reading.
If any of the following symptoms are present, which are alarming in their nature, please call a doctor immediately.
The symptoms are the following:
- Constant vomiting or diarrhoea
- Dry mouth
- Earache or pulling at ears
- Fever comes and goes over several days
- Baby high-pitched crying
- Irritability
- No appetite
- Pale appearance
- Seizures
- Severe headache
- Skin rash
- Sore or swollen joints
- Stiff neck
- Stomach pain
- Swelling of the soft spot on a little one’s head
- Unresponsiveness or limpness
- Wheezing or problems breathing
How does a thermometer work?
A thermometer is a device for accurately measuring temperatures. The two blueprint elements of which the thermometer consists are the following:
- temperature sensor
- some means of converting the physical change in a measurable numerical value
Thermometers are used in many types of industries to control and regulate heat related processes such as the study of weather, medicine, scientific research and so forth.
Different thermometers operate by different principles.
This includes the thermal expansion of solids or liquids with the change of temperature, and the change in the pressure of gas while heating or cooling.
Most metals are good conductors of heat and are in a solid state of aggregation at a room temperature.
Mercury is the only one in a liquid state of aggregation at room temperature and has a high coefficient of expansion.
As such the slightest change of temperature is notable when it’s used in a thermometer.
They can be digital or non-digital.
Baby Monitors
It’s also worth investing in a reliable baby monitor that tracks and sends alerts on their bedroom temperature. This way you can keep an eye on both the environment and the child.
Have a look at this Motorola mbp36s* and see why this is voted the best video monitor for babies.
How to read a thermometer, both digital & non-digital versions
When using a digital thermometer, there shouldn’t have been anything hot or cold in your mouth before starting the measuring process as you may receive an inaccurate reading.
The process for a digital thermometer is the following:
- The thermometer should be removed from its holder
- The thermometer needs to be clean, so washing the tip and disinfecting it is a must
- With mouth open wide, the tip should be placed under the tongue
- Lips should be placed softly on the thermometer
- Keep it like that until it beeps.
- After the beeping, numbers should show on the glass window – that means you can take it out
- The numbers represent the temperature
- If you think it’s necessary, write down your temperature for comparison if you plan to repeat the process soon
- Wash and disinfect the tip again, then place the digital thermometer in its holder
When using a non-digital (glass) thermometer, you should wait at least 10 min before starting the procedure if you have eaten or drank anything hot or cold.
The process for a non-digital version is as follows:
- Remove the thermometer from its holder
- Hold the thermometer on the opposite side of its measuring tip (the opposite of the colored side which can be blue, red, silver, )
- Clean the thermometer with soap and water, then disinfect it with alcohol
- Firmly hold the thermometer in your hand until you see the colored line. The line is supposed to read less than 35.6C (96F). If that is not the case, firmly shake the thermometer sideways with the colored side being on the opposite side of your grip. You should do that over a bed or couch so if it slips it doesn’t break
- After that, check if it reads the correct previously mentioned numerical value. If it does, we are ready to go. If it doesn’t then simply repeat the procedure
- Open your mouth and place the colored side tip under your tongue
- Place your lips gently on the thermometer but don’t bite the glass (this is important!)
- Keep it that way for about 3 minutes, but don’t rush it – if you hold it too short it might show inaccurate readings
- Remove the thermometer from your mouth without touching the tip
- With care, wipe the thermometer with a tissue
- Place the thermometer at eye level
- Turn it slowly until you see the colored line, regardless of its color (blue, red or silver)
- Long marks represent 1 degree, short ones represent 0.2. This way you can see your temperature with satisfying precision
- Write down your temperature if needed if you intend to keep track of your temperature or have an intent to repeat the process soon
- Wash and disinfect the thermometer after you’re done using it. Don’t wash it with warm water as it might break it
- Put it in its holder
Concluding things
And that’s about it! I hope this article proves useful to your needs when it comes to taking care of your child, specifically when dealing with increased body temperatures, fevers or signs of irritability.
We have defined the proper differences from mild body temperature increases, which could be helpful (as it helps the infant build up an immune system) and a serious fever which may require proper medical attention for your little one.
We have also covered the proper means of how the temperature should be measured, the precautions that need to be taken and how to clean and disinfect it after and before the use properly to avoid any contamination.
Having all of this in mind, now you, as a parent should be at ease and have an easier time taking care of your child when he needs you the most.
We wish you nothing but a healthy life and prosperity for you and your family, good luck from all at the Beta Dad Blog!
